Abstract
Background: Autologous hematopoietic stem cell transplantation (AHCT) in the up-front setting is the standard-of-care for newly diagnosed multiple myeloma (NDMM). Contemporary induction regimens generate deeper responses, with higher rates of minimal residual disease (MRD) negativity in the bone marrow (BM) leading to improved progression-free survival (PFS) and overall survival (OS). However, it is unclear whether stem cell autograft (AG) contamination with myeloma cells and/or their precursors contributes to relapse after AHCT. To address this, we examined MM contamination of AG by next-generation flow cytometry (NGF) to determine the predictive value of AG MRD status on outcomes after AHCT.
Methods: This study included 119 NDMM patients with prospectively collected BM and AG MRD results by NGF who underwent stem cell collection and up-front AHCT at our institution between Sept 2017 and Feb 2020. AG MRD status was assessed in peripheral blood at the time of stem cell collection (SCC). BM MRD status was assessed post-induction/pre-SCC and at 3-months post-AHCT. Additional BM MRD results were also available at 1- and 2-years post-AHCT for most patients. Patients were dichotomized based on AG MRD status (negative vs positive). A Kaplan-Meier model compared median PFS and OS between cohorts. A cox proportional hazards model determined prognostic impact, adjusting for high-risk cytogenetics by FISH and induction therapy.
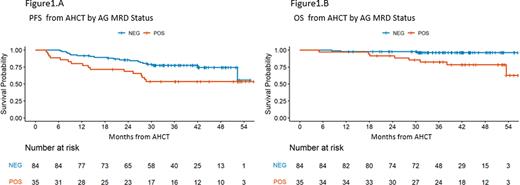
Results: Baseline characteristics were balanced between the MRD-negative and positive groups, with median age at AHCT of 61 (range, 55-67) years in the MRD-negative group and 60 (range, 54-67) years in the MRD-positive group. Patients received a median of 6 (range, 2-12) induction cycles with daratumumab, carfilzomib, lenalidomide, and dexamethasone (D-KRd, n=20), KRd (n=38), bortezomib, lenalidomide, and dexamethasone (VRD, n=51), or other therapy (n=10). Patients with MRD-positive AG were not enriched for high-risk cytogenetics. AG MRD-negativity rates after D-KRd, KRd, VRd, and other therapy were 95.0%, 78.9%, 58.8%, and 50%, respectively. All patients with MRD-positive AG (n=35) also had MRD-positive pre-AHCT BM, whereas 71% of patients with MRD-negative AG had MRD-positive pre-AHCT BM (p <0.001). Sustained or conversion to MRD-negativity in the BM at 3-months and 1-year post-AHCT was observed more for patients with MRD-negative AG than MRD-positive AG (40% vs 9%). At a median follow-up of 40 months (range 33- 46) after AHCT, patients with MRD-negative AG, compared with MRD-positive AG counterparts, had a significantly improved PFS (3-y PFS 78%, CI: 69 ‒ 87, vs. 54%, CI: 39 ‒ 73, p=0.021)(Fig1A) and trend toward better OS (3-y OS 96%, CI: 92 ‒ 100, vs. 82%, CI: 70 ‒ 96)(Fig1B) . The 3-year PFS of the MRD-negative AG group treated with D-KRd, KRd, VRd, and other therapy were 84% (CI: 69 ‒ 100), 79% (CI: 65 ‒ 96), 76% (CI: 71 ‒ 98), and 60% (CI:29 ‒ 100), respectively, while for the MRD-positive AG group treated with KRd, VRd, and other therapy (no D-KRd in this group), 3-year PFS rates were 73% (CI: 47 ‒ 100), 57% (CI: 39 ‒ 83), and 20% (CI:3.5 ‒ 100), respectively (p = 0.4). The 3-year PFS for patients with or without high-risk cytogenetics were 59% (CI: 44 ‒79) and 90% (CI: 81 ‒ 100), respectively, in the MRD-negative AG group, and 40% (CI: 22 ‒ 74) and 67% (CI: 49 ‒ 93), respectively, in the MRD-positive AG group (p = 0.002). The 3-year OS rates were 93% (CI: 85 ‒ 100) and 100% (CI: 100 ‒ 100) for the MRD-negative AG group and 76% (CI: 61 ‒ 100) and 84% (CI: 69 ‒ 100) for the MRD-positive group (p not calculated). On univariate analysis of PFS, the presence of high-risk cytogenetics (HR 3.2, CI: 1.55 ‒ 6.57), R-ISS stage (HR 3.01, CI 1.42 ‒6.41 for R-ISS=3), and AG MRD positive (HR 2.14, CI: 1.10 ‒ 4.16) were significant prognostic factors. Multivariate analysis identified high-risk cytogenetics (HR 3.16, CI: 1.51 ‒ 6.60) as the only significant factor for PFS.
Conclusion: Patients with MRD-negative AG have improved PFS and OS following AHCT. These findings support the potential utility of AG MRD status as a prognostic parameter for clinical outcomes, with implications for guiding post-AHCT therapy.
Disclosures
Nishimura:Chugai Pharmaceutical Co.: Consultancy; JANSSEN PHARMACEUTICAL K.K.: Honoraria; Ono Pharmaceutical Co.: Honoraria. Landau:Karyopharm: Consultancy; Pfizer: Consultancy; Janssen Scientific Affairs, LLC: Other: grants/pending grants; Alexion: Other: grants/pending grants; Memorial Sloan Kettering Cancer Center: Current Employment; Celgene: Consultancy; Juno: Consultancy; Caelum Biosciences: Consultancy; Legend Biotech USA Inc: Consultancy; Janssen: Consultancy; Takeda Pharmaceuticals: Consultancy, Other: grants/pending grants; Prothena: Honoraria. Lahoud:MorphoSys, Inc: Membership on an entity's Board of Directors or advisory committees. Scordo:i3Health (CME): Honoraria; Angiocrine Bioscience, Inc.: Consultancy, Research Funding; Medscape, LCC (CME): Honoraria; McKinsey & Company: Consultancy; Kite - A Gilead Company: Other: Ad-hoc advisory board (past); Amgen, Inc.: Research Funding; Omeros Corporation: Consultancy, Research Funding. Shah:Janssen: Research Funding; Amgen: Research Funding; Beyond Spring: Research Funding. Hassoun:Takeda: Research Funding; Janssen Pharmaceuticals: Research Funding; Celgene: Research Funding. Hultcrantz:Amgen, Daichii Sankyo, Cosette, GSK: Research Funding; Curio Science LLC: Consultancy; Intellisphere LLC: Consultancy; Bristol-Myers Squibb: Membership on an entity's Board of Directors or advisory committees; GSK: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding. Lesokhin:Memorial Sloan Kettering Cancer Center: Current Employment; Pfizer, Genmab, Sanofi, Iteos, BMS, Janssen: Consultancy; BMS: Honoraria; Janssen, Pfizer, BMS, Genentech/Roche: Research Funding; Janssen, Pfizer, Iteos, Sanofi, Genmab: Honoraria; Serametrix, inc: Patents & Royalties; Trillium Therapeutics: Consultancy, Research Funding; Sanofi: Research Funding; Amgen: Honoraria. Mailankody:Evicore: Consultancy; Janssen Oncology: Consultancy, Research Funding; BioAscend: Consultancy; Optum Oncology: Consultancy; Allogene Therapeutics: Research Funding; Takeda Oncology: Research Funding; Juno Therapeutics: Research Funding; Bristol Myers Squibb: Research Funding; Fate Therapeutics: Research Funding; Plexus Communication: Honoraria; OncLive: Honoraria; Physician Education Resource: Honoraria; Legend Biotech: Consultancy; Memorial Sloan Kettering Cancer Center: Current Employment. Shah:Janssen: Consultancy, Research Funding; Bristol Myers Squibb: Consultancy, Research Funding; MashUpMD: Honoraria; ACCC: Honoraria; MJH Lifesciences: Consultancy, Honoraria; Sanofi: Consultancy. Tan:Janssen: Honoraria, Research Funding. Usmani:Abbvie, Amgen, BMS, Celgene, EdoPharma, Genentech, Gilead, GSK, Janssen,Oncopeptides, Sanofi, Seattle Genetics, SecuraBio, SkylineDX, Takeda, TeneoBio: Consultancy; Amgen, BMS, Janssen, Sanofi: Speakers Bureau; Amgen, Array Biopharma, BMS, Celgene, GSK, Janssen, Merck, Pharmacyclics, Sanofi, Seattle Genetics, SkylineDX, Takeda: Research Funding. Giralt:Kite: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees; MILTENYI: Research Funding; TAKEDA: Membership on an entity's Board of Directors or advisory committees, Research Funding; OMEROS: Research Funding; SPECTRUM Pharma: Membership on an entity's Board of Directors or advisory committees; Actinuum: Membership on an entity's Board of Directors or advisory committees, Research Funding; Janssen: Membership on an entity's Board of Directors or advisory committees; Jazz Pharmaceutical: Membership on an entity's Board of Directors or advisory committees; Johnson & Johnson: Membership on an entity's Board of Directors or advisory committees, Research Funding; Amgen: Membership on an entity's Board of Directors or advisory committees, Research Funding; Celgene: Membership on an entity's Board of Directors or advisory committees, Research Funding. Roshal:Celgene: Other: Provision of services; Auron Therapeutics: Other: Ownership / Equity interests; Provision of services; Physicians' Education Resource: Other: Provision of services; NGM: Other: Funding; Beat AML: Other: Funding; Roche: Other: Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal